Why Dual Diagnosis Rehab Programs Are Critical for Lasting Recovery
A dual diagnosis rehab program treats both mental health disorders and substance use disorders simultaneously. This integrated approach is essential because nearly 50% of people with addiction also have a serious mental illness, and treating only one condition often leads to relapse.
What to Look for in a Dual Diagnosis Rehab Program:
- Integrated treatment that addresses both conditions simultaneously
- Evidence-based therapies like CBT, DBT, and trauma-informed care
- Holistic modalities including mindfulness, yoga, and non-invasive detox
- Individualized treatment plans based on comprehensive assessment
- Aftercare support with relapse prevention and peer support groups
The statistics are concerning. An estimated 9.2 million adults in the United States struggle with co-occurring disorders each year. In Texas alone, nearly 37% of adults report anxiety or depression symptoms while 8% have a substance use disorder. Yet only 9.1% of people with co-occurring disorders receive treatment for both conditions.
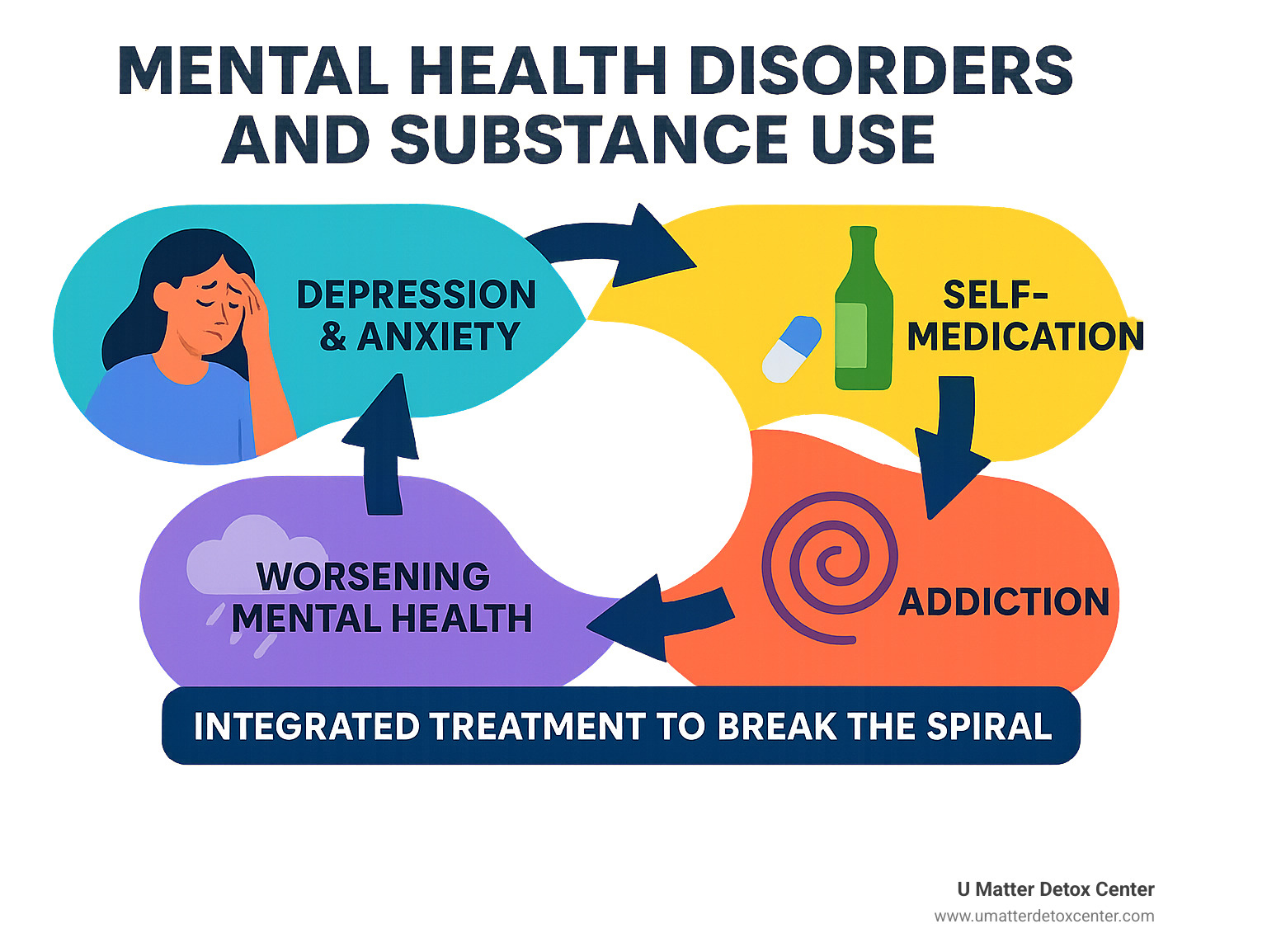
This treatment gap exists because many people don't realize their mental health struggles and substance use are connected. The cycle looks like this: Mental health symptoms cause distress → Substances provide temporary relief → Addiction develops → Mental health worsens → More substances needed → Downward spiral continues.
Breaking this cycle requires treating both the mind and the addiction together. That's where dual diagnosis rehab programs come in.
Understanding Dual Diagnosis: When Mental Health Meets Substance Use
When someone struggles with both a mental health disorder and substance use simultaneously, this is called a dual diagnosis or co-occurring disorders. These aren't separate problems—they're deeply connected, feeding off each other in ways that make recovery challenging.
9.2 million adults in the United States dealt with co-occurring mental illness and substance use disorders in 2020. Among people with addiction, more than 25% also battle mental health conditions.
Several factors create this perfect storm: genetics and family history, trauma and adverse childhood experiences, chronic stress, and social isolation. The relationship works both ways—sometimes depression or anxiety comes first, leading to substance use for coping. Other times, heavy substance use triggers mental health problems.
The self-medication cycle becomes dangerous. Someone with untreated anxiety finds alcohol calms their nerves before social situations. It works initially, but alcohol actually worsens anxiety over time. The brain starts depending on it, creating a cycle where anxiety worsens and drinking becomes necessary just to function.
This is why integrated care makes such a difference. When treatment teams address both addiction and mental health symptoms simultaneously, people have much better outcomes than treating each condition separately.
What Is a Dual Diagnosis Rehab Program?
A dual diagnosis rehab program specifically treats both mental health disorders and substance use disorders simultaneously. Unlike traditional addiction treatment focusing mainly on stopping substance use, dual diagnosis programs recognize you can't successfully treat one without treating the other.
The therapists are trained in both addiction and mental health. Doctors understand how psychiatric medications interact with substance use. The treatment approach considers both aspects of your health through simultaneous treatment, medical detoxification with psychiatric monitoring, and ongoing support throughout the continuum of care.
How Common Are Co-Occurring Disorders?
Research shows roughly 50% of individuals with substance use disorders also experience mental health disorders. Anxiety disorders, depression, and PTSD are among the most common co-occurring conditions. Bipolar disorder, ADHD, and personality disorders also frequently appear alongside addiction.
In Texas, nearly 37% of adults report anxiety or depression symptoms while 8% have a substance use disorder. This means hundreds of thousands of Texans likely struggle with co-occurring conditions, yet only a fraction receive appropriate integrated treatment.
Do I Need a Dual Diagnosis Rehab Program?

If you're asking this question, you're taking an important step toward understanding your health needs. Many people struggle for years without realizing their mental health and substance use issues are deeply connected.
Perhaps you reach for substances when anxiety hits, or depression lingers during sobriety. Maybe you've tried addiction treatment before but relapsed, wondering why traditional approaches didn't work. These experiences often point to co-occurring disorders needing specialized attention.
One challenge is distinguishing between withdrawal symptoms and underlying mental health disorders. Anxiety and depression are common during early recovery, but they might be temporary withdrawal effects rather than separate conditions. Professional assessment becomes crucial to untangle these complex symptoms.
Signs & Symptoms to Watch For
Extreme mood swings unrelated to substance use might indicate an underlying mood disorder. Using alcohol to calm anxiety, stimulants to lift depression, or opioids to numb emotional pain shows a self-medication pattern—one of the strongest indicators of co-occurring disorders.
Risky behavior often escalates when mental health episodes coincide with substance use. Chronic relapse despite sincere efforts to get sober can indicate untreated mental health issues sabotaging recovery.
Trauma history frequently underlies both addiction and psychiatric symptoms. Nightmares, flashbacks, hypervigilance, or feeling constantly on edge might drive substance use for relief.
Assessment & Diagnosis in Rehab Settings
Getting accurate assessment is like having a roadmap for recovery. At U Matter Detox Center, our clinical interview process explores detailed substance use history, mental health symptoms, family background, and trauma experiences.
Standardized assessments help apply DSM-5 criteria for both conditions. The medical evaluation includes toxicology screening, physical examination, and medication review. We assess withdrawal risk and medical complications affecting treatment.
Crucially, we allow time for substances to clear before making final mental health diagnoses. Some symptoms appearing to be depression or anxiety might be withdrawal effects that resolve with sobriety. Ongoing monitoring means we regularly reassess progress and adjust treatment plans.
For detailed information about our approach to addiction and mental health, read our guide on When Addiction Meets Mental Health: Understanding Dual Diagnosis Detox.
Inside a Dual Diagnosis Rehab Program: Integrated Therapies & Modalities
A dual diagnosis rehab program provides comprehensive care recognizing how deeply mental health and addiction are connected. The most effective programs weave together evidence-based clinical treatments with holistic approaches healing your whole person.
Individual therapy becomes the cornerstone with therapists trained in both addiction and mental health. Group therapy connects you with others who understand your struggles. Medication management carefully balances treatments for both conditions, while family therapy helps heal damaged relationships.
Trauma-informed care is essential since most people with co-occurring disorders have experienced trauma. Everything from staff interactions to treatment space design considers trauma's impact on both mental health and substance use.
Core Clinical Interventions
Cognitive Behavioral Therapy (CBT) helps you understand connections between thoughts, feelings, and behaviors. You'll learn to identify triggers setting off both mental health symptoms and substance cravings, developing healthier coping strategies.
Dialectical Behavior Therapy (DBT) teaches four life-changing skills: mindfulness keeps you grounded in the present, distress tolerance provides crisis survival tools, emotion regulation helps manage overwhelming feelings, and interpersonal effectiveness rebuilds healthy relationships.
Eye Movement Desensitization and Reprocessing (EMDR) effectively processes trauma. Many people with dual diagnosis carry painful memories fueling both mental health symptoms and substance use. EMDR helps your brain process these memories safely.
Medication management requires special expertise, coordinating Medication-Assisted Treatment (MAT) for addiction with psychiatric medications for mental health conditions.
Holistic & Non-Invasive Improvements
U Matter Detox Center combines advanced technologies with natural healing processes. Neurofeedback helps retrain brain patterns, reducing anxiety and depression symptoms while improving focus and reducing cravings.
Biofeedback teaches control over body functions affecting mood and cravings. IV therapy provides nutritional support, while infrared sauna sessions help eliminate toxins. Oxygen therapy supports healing and mental clarity.
Acupuncture through the NADA protocol reduces withdrawal symptoms and cravings while alleviating anxiety and depression. Mindfulness and meditation practices become essential long-term tools.
For more information about our holistic approach, explore our guide on What to Expect at a Holistic Detox Center: Therapies, Benefits, and Results.
Art and music therapy provide safe emotional expression, while equine therapy builds trust and emotional regulation. Nature therapy offers grounding and stress relief, and nutritional counseling addresses physical health impacts.
Choosing the Right Dual Diagnosis Rehab Program

Finding the right dual diagnosis rehab program requires understanding what to look for. Not all treatment centers handle co-occurring disorders—you need a program specifically designed for dual diagnosis.
Accreditation matters. Look for programs accredited by The Joint Commission or CARF. Staff qualifications are crucial—the best programs have dual-licensed clinicians trained in both addiction treatment and mental health care.
Insurance coverage has improved dramatically thanks to mental health parity laws. Most major insurance plans now cover dual diagnosis treatment, including private insurance, Medicare, Medicaid, and TRICARE.
Residential vs. Outpatient Dual Diagnosis Rehab Program
Residential programs offer intensive care with 24/7 medical supervision for 30 to 90 days. This immersive environment removes triggers and distractions, allowing complete focus on healing. The peer support aspect is powerful—you're surrounded by others who understand your struggles.
Outpatient programs let you maintain daily routines while receiving treatment. Intensive Outpatient Programs (IOP) typically meet 3-5 days weekly for 3-4 hours. Partial Hospitalization Programs (PHP) are more intensive, meeting 5-7 days weekly for 6-8 hours.
Many people benefit from both—starting with residential treatment for stabilization, then stepping down to intensive outpatient care. This continuum of care approach often provides the best long-term outcomes.
Questions to Ask Before Enrolling
Before committing to any dual diagnosis rehab program, ask the right questions. Start with the assessment process—how comprehensive is their initial evaluation? A thorough assessment is the foundation of effective treatment.
Ask about staff credentials, staff-to-client ratios, and meeting frequency with your primary therapist. Trauma services are crucial—ask specifically about trauma-informed care and available therapies like EMDR.
Don't forget practical matters: insurance acceptance, program length, and aftercare programs. Some facilities offer alumni programs, ongoing support groups, or relapse prevention coaching.
For detailed information about inpatient dual diagnosis treatment, read our guide: Mind Meets Matter: Understanding Inpatient Dual Diagnosis Programs.
Journey Through Treatment: Timeline & Expectations
Knowing what lies ahead can ease worry about entering a dual diagnosis rehab program. Every recovery journey is unique, but there are common stages most people experience.
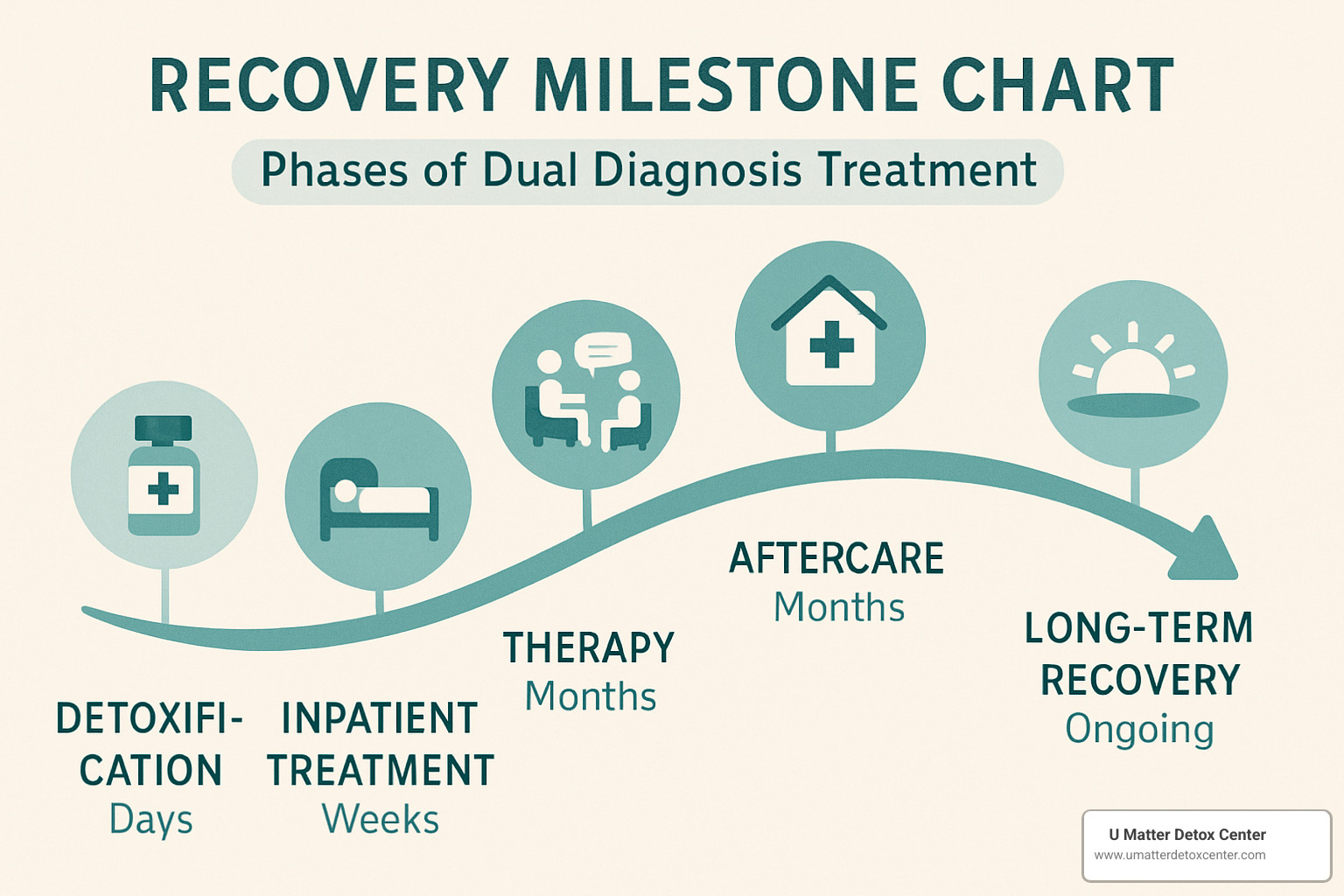
Detoxification (3-10 Days): Your journey begins with safely clearing substances from your body while monitoring mental health. You'll receive round-the-clock medical support, withdrawal symptom medication, and initial psychiatric evaluation.
Residential/Inpatient Treatment (30-90 Days): Comprehensive assessment of mental health and substance use, regular individual and group therapy, medication adjustment, family therapy, and trauma work. Holistic therapies like mindfulness, yoga, and equine therapy support overall wellness.
Step-Down Care (3-12 Months): Treatment becomes less intensive but remains structured through Intensive Outpatient Programs (IOP) or Partial Hospitalization Programs (PHP). Sober living environments and vocational support help transition back to everyday life.
Long-Term Recovery (Ongoing): Regular therapy sessions, psychiatric check-ins, and peer support groups become part of ongoing plans. Alumni groups and relapse prevention coaching maintain connection and motivation.
Addressing Trauma Along the Way
Trauma affects up to 90% of people in addiction treatment. Healing approaches include EMDR for processing painful memories, somatic therapies for trauma stored in the body, and expressive therapies when words aren't enough.
Physical and emotional safety are priorities through predictable routines, cultural respect, and peer support in safe healing spaces.
Sustaining Long-Term Recovery
Long-term recovery means building a life you love through ongoing support for both mental health and substance use recovery. Peer communities like Dual Diagnosis Anonymous offer vital connection and hope.
Building practical skills includes money management, job hunting, self-care, healthy relationships, and stress management. Regular exercise, nutrition, sleep routines, and mindfulness help maintain stability.
For more details on holistic therapies, check out What to Expect at a Holistic Detox Center: Therapies, Benefits, and Results.
Frequently Asked Questions About Dual Diagnosis Rehab Programs
Why is it risky to treat only addiction or only mental health?
Imagine trying to fix a car with two flat tires by only replacing one. You might get rolling again, but you won't get very far before breaking down. That's essentially what happens when we treat addiction without addressing mental health, or vice versa.
When addiction treatment ignores mental health, the underlying emotional pain remains untouched. Someone might successfully detox from alcohol, but if their depression goes untreated, they're likely to return to drinking as a way to cope. The stress, anxiety, or trauma that contributed to their substance use in the first place becomes a ticking time bomb for relapse.
When mental health treatment overlooks addiction, it's like trying to have a conversation with someone who's not fully present. Ongoing substance use interferes with therapy progress, makes medications less effective, and keeps the person from developing genuine coping skills. The substances continue to worsen the very mental health symptoms they're trying to treat.
Research consistently shows that integrated treatment through a dual diagnosis rehab program leads to better outcomes across the board. People stay in treatment longer, have lower relapse rates, and report better quality of life. It's not just more effective—it's more cost-effective too, reducing the need for repeated treatment episodes and emergency interventions.
The bottom line? Both conditions feed off each other. Breaking this cycle requires addressing both simultaneously, which is exactly what dual diagnosis treatment does.
Are dual diagnosis services usually covered by insurance or Medicaid?
Here's some good news: dual diagnosis treatment is typically covered by insurance, thanks to federal laws that require equal coverage for mental health and addiction treatment. The Mental Health Parity and Addiction Equity Act and the Affordable Care Act have made dual diagnosis care much more accessible.
Most insurance plans cover the full spectrum of dual diagnosis services, including detoxification, residential treatment, outpatient therapy, medication management, and psychiatric services. This includes private insurance plans (PPO, HMO, EPO), Medicare for those 65 and older, Medicaid for qualifying individuals and families, and TRICARE for military families.
Medicaid coverage has expanded significantly since the Affordable Care Act, making dual diagnosis treatment available to many who previously couldn't afford it. Medicaid typically covers all levels of care, from detox through long-term support services.
At U Matter Detox Center, we work with most major insurance providers to make treatment accessible. We handle the insurance verification process and help you understand your benefits, including any deductibles or co-payments you might be responsible for.
The key is getting pre-authorization when required and keeping detailed records of all communications with your insurance company. If coverage is initially denied, don't give up—many denials can be successfully appealed with the right documentation.
How can families support loved ones during and after rehab?
Family support can make or break someone's recovery from co-occurring disorders. But here's the thing—good intentions don't always translate to helpful actions. The most loving thing you can do is learn how to support effectively.
During treatment, your role is to be present without being intrusive. Participate in family therapy sessions when invited, attend educational programs to understand dual diagnosis, and maintain healthy boundaries while showing support. This means avoiding the urge to "fix" everything or enable behaviors that might undermine treatment.
After treatment, your loved one will need ongoing support as they steer the real world with new coping skills. Continue family therapy to work on relationship healing, learn about their specific triggers, and support healthy activities and routines. Encourage their ongoing treatment and support group attendance, but recovery is their responsibility, not yours.
A challenge families face is managing their own emotions—guilt, anger, fear, and frustration are all normal. You might blame yourself or feel like you're walking on eggshells. This is why many families benefit from their own support groups like Al-Anon or NAMI, where they can process these feelings with others who understand.
Recovery isn't linear, and there may be setbacks along the way. Having realistic expectations about the timeline and celebrating small victories can help maintain hope during difficult moments. Your loved one's recovery journey is ultimately theirs to walk, but having a supportive family can make all the difference in their success.
Conclusion

Recovery from co-occurring disorders is absolutely possible, and you don't have to do it alone. Every day, people break free from the exhausting cycle of mental health symptoms and substance use by choosing integrated treatment addressing both conditions together.
At U Matter Detox Center, we've seen countless people transform their lives through our integrated approach. We understand that your mental health and addiction aren't separate problems requiring separate solutions. They're interconnected challenges needing treatment together, with compassion, expertise, and the right combination of evidence-based and holistic therapies.
What makes our approach different is that we truly believe you matter—not just your addiction or mental health symptoms, but you as a whole person. We combine advanced non-invasive detox technologies with natural healing methods and proven therapeutic interventions, creating individualized treatment plans based on comprehensive assessment of your unique needs.
Our luxury, holistic environment creates a space where healing happens naturally. When you're surrounded by beauty and comfort, treated with dignity and respect, with access to innovative therapies alongside traditional treatments, recovery becomes not just possible but sustainable.
The statistics showing only 9.1% of people with co-occurring disorders receive treatment for both conditions don't have to include you. Insurance coverage is available for most people, and the support you need is here when you're ready.
Whether you're struggling with depression and alcohol, anxiety and prescription medications, trauma and substance abuse, or any other combination, your story doesn't have to end here. This could be where your real story begins—the story of recovery, healing, and hope.
Recovery isn't just about stopping substance use. It's about waking up with energy and purpose, having difficult conversations without reaching for substances, feeling emotions without being overwhelmed, rebuilding trust with loved ones, and learning to trust yourself again.
Take the first step today. Contact U Matter Detox Center to learn more about our dual diagnosis programs and find how we can help you start your integrated healing journey. Your mind matters, your recovery matters, and you matter. Let us help you heal both your mental health and your relationship with substances—together.
Contact us today to begin your journey toward lasting recovery and mental wellness. Because when you're ready to heal, we're ready to help.

