When Mental Health and Addiction Collide: The Critical Need for Integrated Care
Detox dual diagnosis treatment addresses the complex challenge of treating both substance use disorders and mental health conditions simultaneously. When someone struggles with addiction alongside depression, anxiety, PTSD, or other mental health issues, traditional detox programs often fall short because they only treat one piece of the puzzle.
What You Need to Know About Detox Dual Diagnosis Treatment:
- Definition: Simultaneous treatment of substance withdrawal and co-occurring mental health disorders
- Who Needs It: Nearly 50% of people with addiction also have a mental health condition
- Key Difference: Integrated care treats both conditions together, not separately
- Success Rate: Integrated treatment shows consistently superior outcomes compared to treating disorders individually
- Timeline: Typically 5-14 days for detox phase, with ongoing mental health support
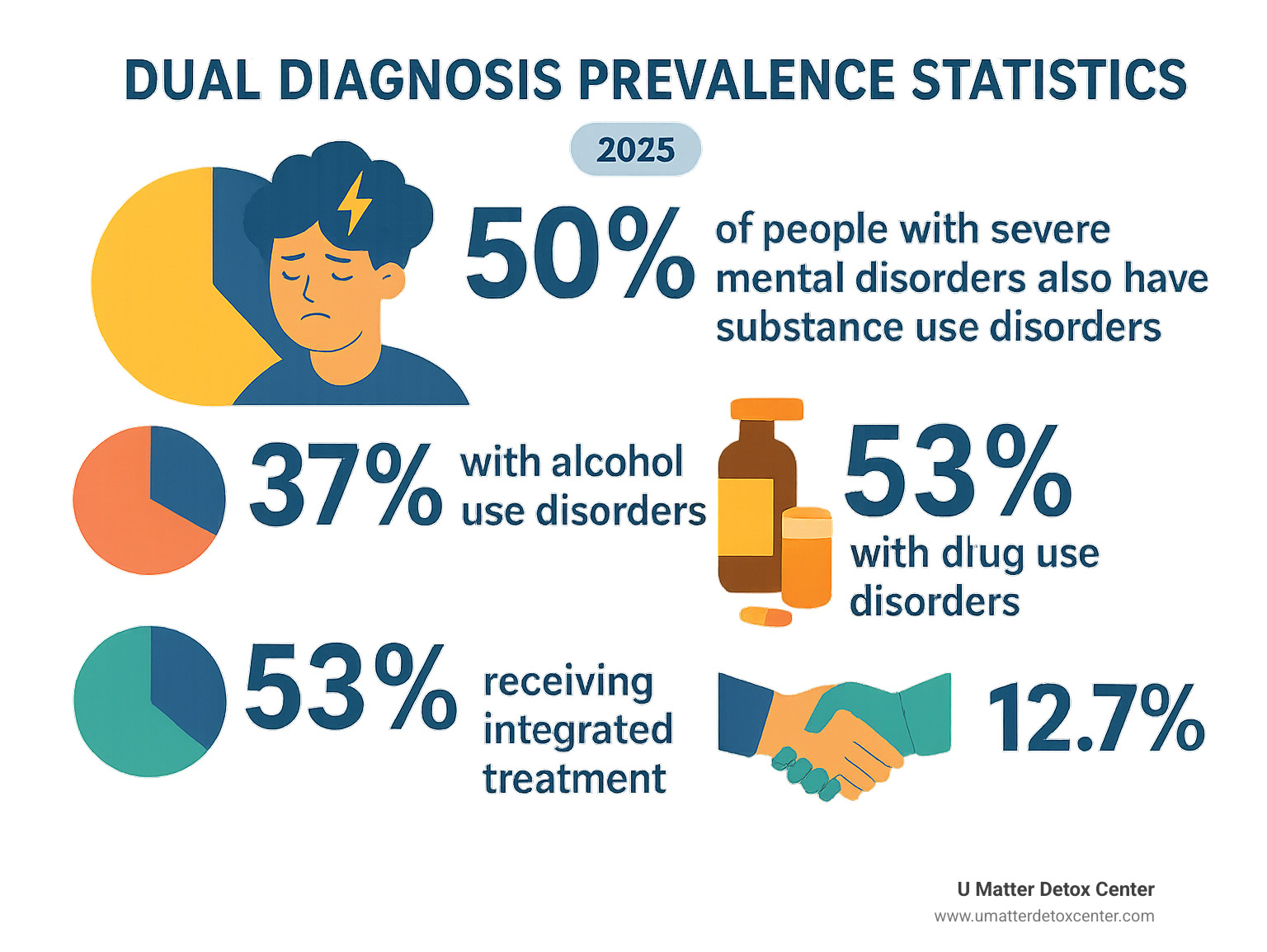
The statistics are striking. Research shows that 9.5 million American adults experienced co-occurring disorders in 2019, yet only 12.7% received treatment for both conditions. This treatment gap explains why so many people cycle through failed recovery attempts.
The challenge is real: substance use can mask mental health symptoms, while untreated mental illness often drives continued addiction. Without addressing both simultaneously, recovery remains elusive for many who've tried traditional approaches without success.
Why This Guide Matters
If you're researching dual diagnosis detox for yourself or a loved one, understanding your options is crucial because the wrong approach can mean the difference between lasting recovery and another cycle of relapse.
This guide breaks down everything you need to know about detox dual diagnosis treatment, from what to expect during the process to how to find the right program. We'll explore evidence-based approaches that work, helping you make informed decisions during what may be one of the most challenging times in your life.
Dual Diagnosis 101: Where Mental Health and Addiction Overlap
Picture this: someone starts drinking wine every night to quiet their racing thoughts from anxiety. What begins as occasional relief gradually becomes a daily necessity. Before long, they need alcohol to function, but their anxiety has gotten worse, not better. They're caught in a cycle where each problem feeds the other.
This is the reality of dual diagnosis – when mental health struggles and addiction become tangled together in ways that make both conditions harder to treat. It's incredibly common, yet many people don't realize they're dealing with two separate issues that need attention.
The numbers tell a powerful story. Research shows that 27% of people have at least one psychiatric disorder, and 45% of people with psychiatric conditions actually have two or more disorders. When substance use enters the picture, the complexity grows exponentially.
What Is a Dual Diagnosis?
A dual diagnosis happens when someone meets the clinical criteria for both a substance use disorder and one or more mental health conditions at the same time. Common dual diagnosis combinations include depression paired with alcohol use disorder, anxiety disorders alongside benzodiazepine dependence, PTSD with opioid addiction, bipolar disorder combined with cocaine use, or schizophrenia occurring with cannabis use disorder.
The famous Kessler survey revealed something striking: people with mental health issues are four times more likely to develop a substance use disorder. This statistic shows how mental health conditions create vulnerability to addiction, often as people desperately try to manage symptoms that feel overwhelming.
What makes dual diagnosis particularly tricky is how each condition can hide or mimic symptoms of the other. Depression might look like withdrawal symptoms, while anxiety could seem like the effects of stimulant use.
Why Integrated Treatment Works
Traditional treatment approaches often tackle addiction and mental health separately. It's like trying to fix a car's engine while completely ignoring a broken transmission – both problems need attention, and they affect each other in ways that make treating them in isolation less effective.
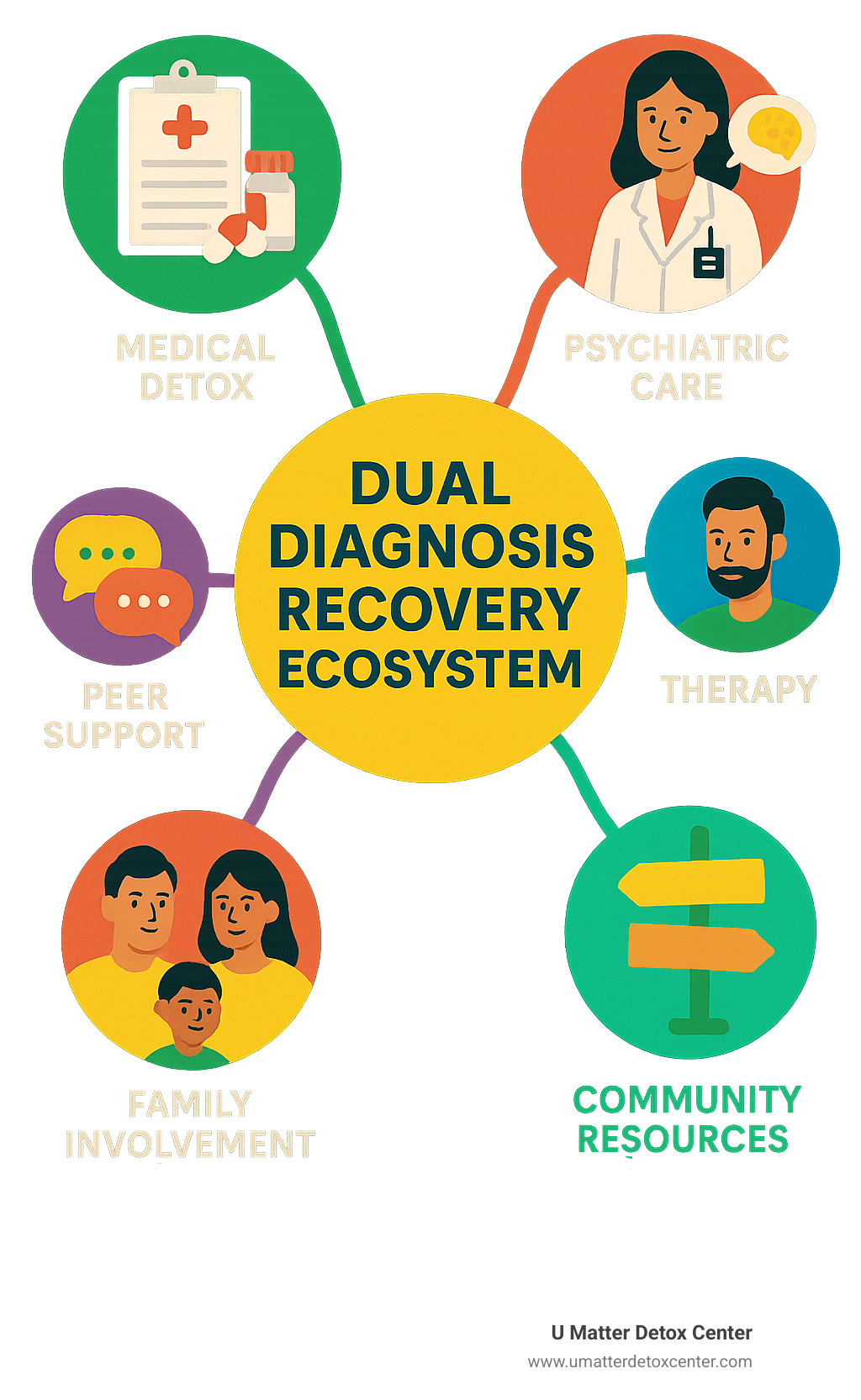
Integrated Dual Disorder Treatment uses the same clinical team and location to address both conditions simultaneously. This approach has consistently shown superior results compared to treating disorders separately. When your therapist understands both your addiction patterns and your mental health triggers, they can help you see connections you might miss on your own.
The beauty of detox dual diagnosis treatment is that it addresses the whole person from day one, recognizing that lasting recovery requires treating both the addiction and the underlying mental health conditions that may have contributed to substance use in the first place.
Detox Dual Diagnosis Treatment: What to Expect

Walking into detox dual diagnosis treatment can feel overwhelming, but knowing what to expect helps ease those first-day nerves. Unlike standard detox programs that focus solely on getting substances out of your system, dual diagnosis treatment recognizes that your mental health needs just as much attention as your physical withdrawal symptoms.
The intake process begins with a comprehensive assessment that looks at your whole story. The clinical team wants to understand not just what substances you've been using, but how your mental health and addiction have been dancing together. This 360-degree assessment examines your substance use patterns, mental health history, medical conditions, family dynamics, and support systems.
Once you're in the program, you'll notice the difference immediately. The staff is watching for signs that your depression might be deepening as alcohol leaves your system, or that your anxiety might spike during stimulant withdrawal. This dual focus on both physical and psychiatric symptoms is what makes detox dual diagnosis treatment so much more comprehensive.
Unique Challenges During Detox
Detox dual diagnosis treatment comes with complications that catch many people off guard. As substances leave your system, mental health symptoms that have been masked or suppressed often surface with surprising intensity. Someone who thought they just had a drinking problem might find they've been self-medicating severe depression for years.
Suicidal ideation becomes a serious concern during this vulnerable time. As the substances that have been numbing emotional pain are removed, some people experience intense psychological distress. This isn't a character flaw or weakness—it's a predictable medical response that requires immediate psychiatric support.
Medication interactions add another challenge. If you're taking psychiatric medications, the detox process can affect how these medications work in your system. Your prescriptions might need adjustment as your body chemistry changes, which is why having both medical doctors and psychiatrists involved is crucial.
Stages of Detox Dual Diagnosis Treatment
The assessment phase typically takes 24 to 48 hours and involves meeting with multiple specialists. Medical doctors examine your physical health and withdrawal risks, while psychiatrists assess your mental health conditions and suicide risk.
During the stabilization phase, which usually lasts 3 to 10 days, the focus shifts to keeping you safe and comfortable while your body and mind adjust. Medications might be used to ease withdrawal symptoms, stabilize your mood, or manage anxiety.
The transition phase happens in the final 1 to 3 days when acute withdrawal symptoms are subsiding. Now the team focuses on preparing you for what comes next. You'll learn about your conditions, develop coping strategies, and create a plan for ongoing treatment. More info about trauma-informed detox services can provide additional support during this critical transition period.
Medically Managed Detox Dual Diagnosis Treatment
Medical management in dual diagnosis detox goes far beyond checking your blood pressure and heart rate. Your care team includes physicians trained in addiction medicine, psychiatrists who understand how substances interact with mental health conditions, psychiatric nurses who can spot early warning signs, and mental health counselors.
24/7 nursing means someone with specialized training is always available to assess both your physical and psychiatric symptoms. Taper plans for substances must be carefully coordinated with any psychiatric medications you're taking, creating individualized schedules that prioritize both safety and mental health stability.
Gold-Standard Therapies & Medications for Dual Diagnosis Detox

When it comes to detox dual diagnosis treatment, the therapies and medications that work aren't just good—they're backed by solid research and real-world results. Think of these evidence-based approaches as your recovery toolkit, each designed to address different pieces of the dual diagnosis puzzle.
Cognitive Behavioral Therapy (CBT) helps you understand the connection between your thoughts, feelings, and behaviors—both the addiction patterns and the mental health symptoms. It's like having a roadmap that shows you exactly how your mind works and where the detours into substance use typically happen.
Dialectical Behavior Therapy (DBT) takes a different angle, focusing on emotional regulation and distress tolerance. If you've ever felt like your emotions were driving the bus while you were just along for the ride, DBT teaches you how to get back in the driver's seat.
Motivational Interviewing (MI) recognizes something important: change is hard, and feeling ambivalent about it is completely normal. When you're facing both addiction and mental health challenges, the idea of tackling both can feel overwhelming. MI helps you find your own reasons for change rather than having someone else's motivation imposed on you.
Evidence-Based Psychotherapies
CBT for Substance Use Disorders (CBT-SUD) gets specific about the relationship between thinking patterns and substance use. What makes this approach particularly effective in dual diagnosis situations is how it addresses the overlapping thought patterns that fuel both addiction and mental health symptoms.
Seeking Safety was designed specifically for people dealing with both PTSD and substance use disorders. Rather than treating symptoms in isolation, Seeking Safety addresses the underlying trauma that may be driving both the mental health symptoms and the substance use.
Eye Movement Desensitization and Reprocessing (EMDR) might sound a bit unusual, but it's remarkably effective for processing traumatic memories. Many people find that once they've processed the trauma that's been haunting them, both their mental health symptoms and their urge to use substances decrease significantly.
Role of Medication in Dual Diagnosis Detox
Medication management during detox dual diagnosis treatment requires a delicate balance. You need medications that can safely manage withdrawal symptoms while also addressing mental health conditions that may become more apparent as substances leave your system.
Buprenorphine serves double duty for people with opioid use disorder and depression. It helps manage opioid withdrawal while also having mood-stabilizing effects. Naltrexone works differently, blocking opioid receptors and reducing alcohol cravings, and it's generally safe for people with most mental health conditions.
For people with bipolar disorder, mood stabilizers like lithium or lamotrigine might be continued or carefully initiated during detox. Antipsychotics become essential for people with schizophrenia or severe mood disorders with psychotic features.
SSRIs and other antidepressants require careful timing considerations. Sometimes it's better to wait until acute withdrawal symptoms pass before starting or adjusting these medications. This is where having psychiatrists who specialize in addiction medicine makes all the difference.
Crafting Your Integrated Recovery Plan
Your detox dual diagnosis treatment journey doesn't end when you leave the detox facility—in many ways, it's just beginning. Creating a solid recovery plan that addresses both your mental health and addiction is like building a bridge to your new life.
The beauty of integrated recovery planning is that it recognizes you're not just someone with addiction, and you're not just someone with a mental health condition. You're a whole person with dreams, relationships, and a life worth living.
During your detox, social workers become your advocates and connectors. Case managers act like your personal GPS through the sometimes confusing world of healthcare. They make sure your psychiatrist knows what your addiction counselor is doing, and vice versa.
Peer support specialists bring something unique to your team—they've walked this path themselves. They understand what it's like to feel hopeful one day and discouraged the next. Their lived experience combined with their training creates a special kind of support that complements professional treatment.
Support Groups & Peer Networks
Finding your tribe in recovery can be life-changing, especially when you're dealing with both addiction and mental health challenges. The isolation that often comes with dual diagnosis starts to lift when you connect with others who truly understand your experience.
12-Step programs like Alcoholics Anonymous and Narcotics Anonymous are everywhere, which is both their strength and limitation. They're incredibly accessible and have helped millions of people, but they don't specifically address mental health issues.
SMART Recovery takes a more scientific approach that appeals to people who like evidence-based strategies. Instead of focusing on powerlessness, SMART Recovery emphasizes building motivation, developing coping skills, and creating a balanced life.
Double Trouble in Recovery groups were created specifically for people like you—those managing both addiction and mental health conditions. These meetings understand that your depression isn't a character flaw and your anxiety isn't something you can just "get over."
Aftercare & Relapse Prevention
Here's the truth about dual diagnosis recovery: both conditions are chronic, which means they require ongoing attention. But chronic doesn't mean hopeless—it means manageable with the right support and strategies.
Your aftercare plan becomes your roadmap for navigating life's inevitable challenges without returning to old coping mechanisms. Trigger management is a crucial part of this plan because triggers for substance use and mental health symptoms often overlap.
Relapse prevention for dual diagnosis means watching for warning signs in both areas. The earlier you catch these patterns, the easier they are to address. More info about aftercare planning can help you understand all the continuing care options available to support your long-term recovery.
Finding the Right Dual Diagnosis Detox Program
Choosing the right detox dual diagnosis treatment program can feel overwhelming when you're already dealing with so much. The good news is that quality programs exist, and knowing what to look for can help you find one that truly meets your needs.
Not every detox center handles dual diagnosis well. Some treat addiction and mental health as separate issues, which we now know doesn't work as effectively. You want a program that sees the whole you, not just individual symptoms that need fixing.
Start by looking for centers that specifically mention dual diagnosis or co-occurring disorders in their marketing materials. The clinical team should include both addiction specialists and mental health professionals working as one coordinated unit.
Accreditation matters more than fancy amenities. Look for programs accredited by The Joint Commission or CARF (Commission on Accreditation of Rehabilitation Facilities). These organizations have strict standards for safety and quality of care.
Evidence-based treatment should be clearly explained, not hidden behind vague promises. Quality programs will tell you exactly which therapies they use and why.
Key Questions to Ask Providers
When you call potential programs, don't be shy about asking detailed questions. Good programs welcome informed patients and families who want to understand their approach.
Staff credentials are crucial. Ask if they have psychiatrists available 24/7, not just during business hours. Mental health crises don't follow a schedule. Find out what training their mental health counselors have and whether they specialize in dual diagnosis treatment.
Ask about medication management for both conditions. Someone needs to coordinate your psychiatric medications with any medications used during detox. This requires expertise in both areas, not just good intentions.
Family involvement can make a huge difference in recovery success. Programs that educate families about dual diagnosis and provide ongoing support tend to have better outcomes.
Accessing Services & Funding Options
Insurance coverage for dual diagnosis treatment has improved significantly thanks to mental health parity laws. These laws require insurance companies to cover mental health and addiction treatment at the same level as medical conditions.
Many quality programs have financial counselors who can help steer insurance approval and explore payment options. Don't assume you can't afford treatment without first talking to someone who understands the system.
Government programs may provide funding, especially if you have limited income. Referrals from healthcare providers often carry weight with treatment programs and insurance companies.
Don't let financial concerns stop you from getting help. Many programs offer sliding-scale fees or payment plans. The cost of not getting proper treatment—in terms of health, relationships, and lost opportunities—far exceeds the investment in quality dual diagnosis care.
Frequently Asked Questions about detox dual diagnosis treatment
When you're considering detox dual diagnosis treatment, it's natural to have questions. These are some of the most common concerns we hear from people and their families as they steer this important decision.
How long does detox dual diagnosis treatment take?
The honest answer is that detox dual diagnosis treatment timelines vary quite a bit from person to person. Most people can expect the acute detox phase to last 5-14 days, but this is really just the foundation of your recovery journey, not the finish line.
Alcohol and benzodiazepine withdrawal often require the longest timelines because these substances can be dangerous to stop suddenly. A gradual, medically supervised taper keeps you safe while allowing your mental health symptoms to stabilize.
Mental health condition severity plays a big role in timing too. If you've been using substances to manage severe depression, anxiety, or trauma symptoms, those underlying issues need attention once the substances are removed.
The variability exists for good reason. Rushing through detox when you have dual diagnosis can actually be counterproductive or even dangerous. Your treatment team wants to make sure both your physical withdrawal and mental health symptoms are properly stabilized before you move to the next phase of recovery.
What therapies work best during detox dual diagnosis treatment?
The most effective therapies during detox dual diagnosis treatment are those designed to work with people in early recovery while addressing both conditions at once.
Cognitive Behavioral Therapy (CBT) stands out because it helps you understand the connections between your thoughts, feelings, and behaviors. Even during detox, you can start recognizing patterns like using alcohol when anxious or turning to stimulants when depressed.
Medication-Assisted Treatment (MAT) can be life-changing for people with opioid or alcohol use disorders, especially when you also have mental health conditions. The key is having providers who understand both addiction medicine and psychiatry.
Motivational Interviewing (MI) addresses something many people with dual diagnosis experience: feeling completely overwhelmed by the idea of tackling both addiction and mental health. MI helps you find your own reasons for change rather than feeling pressured by others.
How can families support loved ones in detox dual diagnosis treatment?
Supporting someone through detox dual diagnosis treatment requires a delicate balance of love, boundaries, and education. Many families feel helpless or confused about how to help, especially when previous attempts at support haven't worked.
Education really is the foundation of effective family support. When you understand that dual diagnosis involves two medical conditions affecting the brain, it becomes easier to respond with compassion rather than frustration.
Setting boundaries becomes more nuanced with dual diagnosis. You want to support recovery from both conditions without enabling continued substance use or mental health avoidance.
Visitation guidelines during detox exist for good reasons, even though they can feel harsh. The early days of detox require intense focus on medical and psychiatric stabilization. Following your treatment center's guidelines shows respect for the recovery process and helps ensure the best possible outcome.
Conclusion
Finding the right detox dual diagnosis treatment can feel like searching for a needle in a haystack, especially when you're already overwhelmed by the challenges of managing both addiction and mental health conditions. But here's the truth that gives us hope: integrated treatment works, and recovery is absolutely possible.
The journey through dual diagnosis recovery isn't just about getting clean or managing symptoms—it's about refinding who you are when both your mind and body are working together instead of against each other. Many of our clients describe it as finally feeling like themselves again after years of battling conditions that seemed to feed off each other.
At U Matter Detox Center, we've seen how transformative integrated care can be. Our holistic dual diagnosis programs recognize that your addiction and mental health condition didn't develop in isolation, so they shouldn't be treated that way either. We combine advanced non-invasive technologies with natural remedies to provide the kind of deep, individualized detox that addresses your whole person.
What makes our approach different is that we don't just treat symptoms—we help you understand the connections between your mental health and substance use. Our multidisciplinary team includes addiction medicine physicians, psychiatrists, and licensed therapists who actually talk to each other and coordinate your care.
Located throughout Los Angeles County, from Beverly Hills to Malibu, we bring comprehensive dual diagnosis care directly to your community. Our luxury facilities provide a healing environment where you can focus entirely on recovery without the distractions and stressors of daily life.
The statistics we've shared throughout this guide—like the fact that nearly 50% of people with addiction also have mental health conditions—aren't just numbers. They represent real people who, like you, deserve treatment that addresses their complete experience.
Recovery from dual diagnosis often means letting go of the shame that comes with having multiple conditions that society doesn't always understand. It means learning that needing help for both addiction and mental health isn't a sign of weakness—it's a sign of courage and self-awareness.
If previous treatment attempts have left you feeling hopeless, those programs may not have addressed both conditions simultaneously. Detox dual diagnosis treatment that truly integrates care can break the cycle of relapse and failed attempts that happens when only part of the problem gets addressed.
The path forward starts with a single decision: choosing integrated care that honors the complexity of your experience. More info about holistic dual diagnosis programs can help you understand exactly how our approach might work for your specific situation.
Your recovery matters. Your mental health matters. You matter. And the comprehensive, compassionate care you deserve is available right here in Southern California, often covered by insurance so financial barriers don't stand in your way.
The integrated treatment you need isn't just a dream—it's a reality that's helped thousands of people reclaim their lives. Today could be the day you take that first step toward the recovery you've been searching for.


