Why Inpatient Dual Diagnosis Treatment Is Critical for Complex Recovery
Inpatient dual diagnosis treatment addresses the simultaneous presence of a substance use disorder and a mental health condition in a residential setting. This integrated approach treats both conditions together rather than separately.
Key Facts About Inpatient Dual Diagnosis:
- 17 million adults in the U.S. struggled with co-occurring disorders in 2020
- Only 12.7% of people with dual diagnosis received treatment for both conditions
- 50% of people with substance use disorders will also experience a mental health disorder
- 24/7 medical supervision provides safety during withdrawal and stabilization
- Integrated treatment is more effective than treating conditions separately
When someone experiences both addiction and mental illness, the conditions often fuel each other in a destructive cycle. You might use substances to self-medicate anxiety or depression, only to find that the substances worsen your mental health symptoms over time.
This creates what researchers call a "vicious cycle" - untreated mental health issues worsen substance use, while continued substance use makes mental health symptoms harder to manage. Breaking this cycle requires specialized care that addresses both issues simultaneously.
For high-achieving professionals, the stakes feel even higher. Past treatment failures, privacy needs, and career concerns can delay getting help. But inpatient dual diagnosis programs offer the intensive, comprehensive care needed when outpatient treatment hasn't worked.
The integrated approach means your treatment team - psychiatrists, addiction counselors, and therapists - work together on one unified plan. Instead of juggling separate appointments and conflicting advice, you get coordinated care that makes sense.
Inpatient Dual Diagnosis Explained
When life feels like you're fighting two battles at once - battling addiction while struggling with depression, anxiety, or another mental health condition - you're not alone. Inpatient dual diagnosis care exists precisely because these battles are often interconnected.
Your brain doesn't separate your addiction from your mental health. They're interconnected, feeding off each other in ways that can feel overwhelming. That's why treating them together, rather than as separate problems, makes so much more sense.
The term "dual diagnosis" simply means you meet the criteria for both a substance use disorder and a mental health condition simultaneously. These combinations are incredibly common - up to 50% of people with substance use disorders will also experience a mental health disorder during their lives.
What makes this particularly tricky is figuring out which came first. Often, it doesn't matter. What matters is that both conditions share similar risk factors like genetics, past trauma, and life stressors.
During assessment, clinicians use comprehensive psychiatric evaluations and the DSM-5 diagnostic framework to understand your unique situation. Many programs recommend a period of abstinence before making final mental health diagnoses because substances can create symptoms that look exactly like psychiatric disorders.
| Inpatient vs Outpatient Dual Diagnosis Care |
|---|
| Inpatient: 24/7 medical supervision, intensive daily therapy, protected environment, medical detox available |
| Outpatient: Flexible scheduling, maintain work/family responsibilities, lower cost, requires strong support system |
Defining inpatient dual diagnosis care
Inpatient dual diagnosis care means you live at the treatment facility while receiving round-the-clock care for both your addiction and mental health condition. It's not just about having both services under one roof - it's about having them work together as one unified treatment plan.
This approach follows the brain-disease model. Both addiction and mental illness involve real changes in how your brain functions. When you treat them simultaneously, you're addressing the underlying chemical imbalances that contribute to both conditions.
Instead of bouncing between separate appointments with different providers, you get one coordinated team. Your psychiatrist, addiction counselor, and therapist all work together, sharing insights and adjusting your treatment based on how you respond to different interventions.
Who benefits from inpatient dual diagnosis programs
Sometimes outpatient treatment just isn't enough, especially when you're dealing with complex, interconnected conditions. Several factors indicate that inpatient dual diagnosis treatment might be the right choice.
Safety concerns top the list. If you're having suicidal thoughts, experiencing severe withdrawal symptoms, or dealing with psychotic episodes, you need 24/7 medical monitoring. The same goes if you have a history of seizures or delirium tremens during withdrawal.
Your treatment history also matters. If you've tried outpatient programs multiple times without success, or if you keep relapsing when only one condition gets treated, inpatient care offers the intensive support you need.
The complexity of your situation plays a role too. Using multiple substances, having severe mental health symptoms, or dealing with additional issues like eating disorders or trauma history can make recovery more challenging.
Environmental factors can't be ignored either. If your living situation isn't supportive or substances are easily accessible, removing yourself from those triggers becomes crucial for successful treatment.
Inside the Program: Admission, Therapies & Medication
Starting your journey in an inpatient dual diagnosis program might feel daunting, but knowing what lies ahead can ease those first-day jitters. Most people arrive when they've noticed warning signs that outpatient care isn't sufficient anymore.
These signs often show up as extreme mood swings, inability to control emotions, declining work performance, legal troubles, difficulty maintaining relationships, or using substances just to feel normal - not to get high, but just to function.
The beauty of inpatient dual diagnosis care lies in its 24/7 monitoring. This isn't about being watched constantly - it's about having skilled medical staff available whenever withdrawal symptoms spike, medication needs adjusting, or psychiatric crises emerge.
What's particularly innovative about modern dual diagnosis care is how medical detox happens alongside psychiatric stabilization. While your body clears substances, your treatment team simultaneously stabilizes mood swings, anxiety, or other mental health symptoms.

The therapeutic environment balances individual therapy sessions where you can dive deep into personal triggers and trauma, with group therapy that connects you with others walking similar paths. Holistic modalities and trauma-informed approaches weave throughout the program, recognizing that healing happens on multiple levels.
For a deeper understanding of how these elements come together, explore our 30-Day Detox Program, which seamlessly integrates medical detox with mental health stabilization.
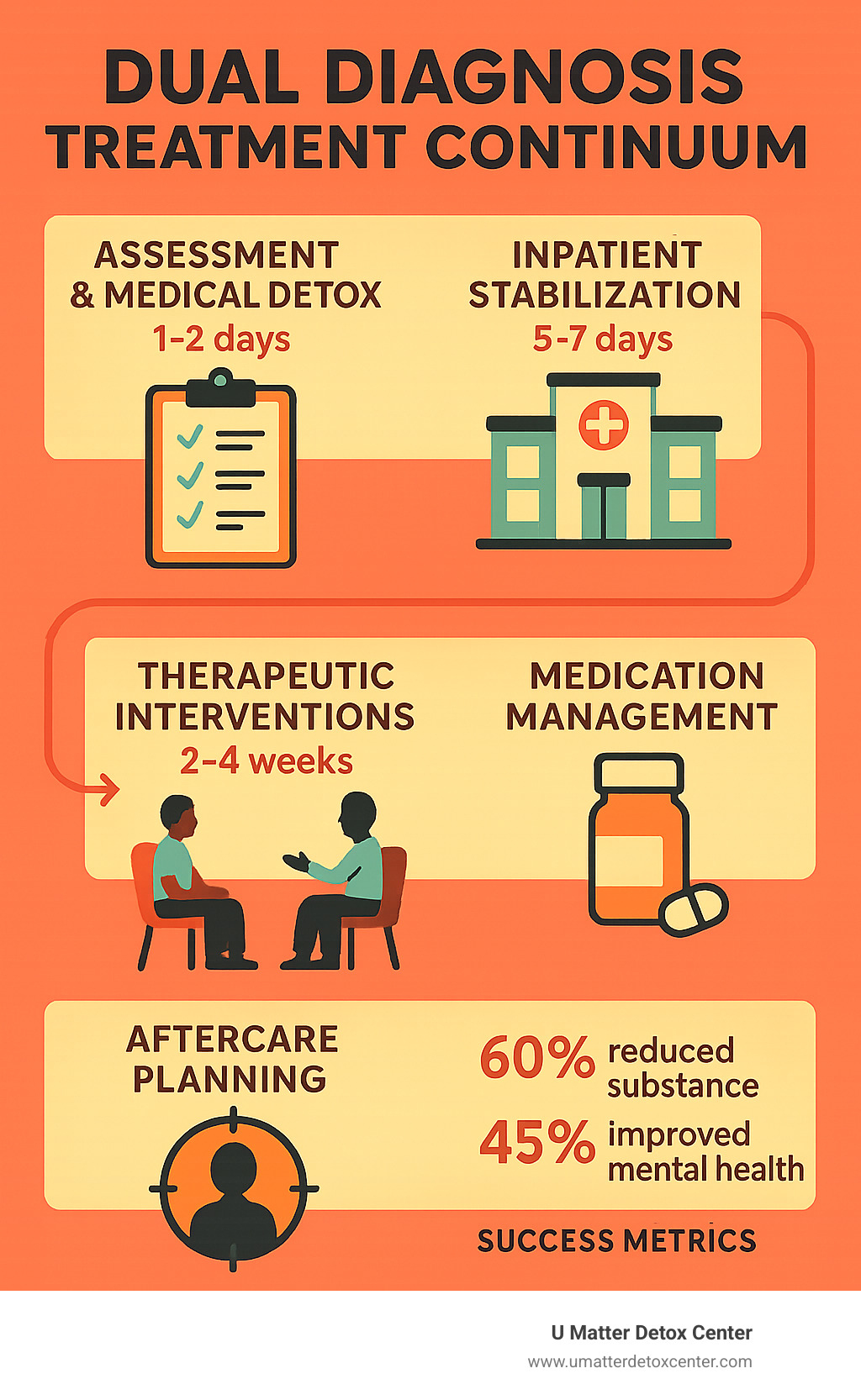
Comprehensive assessment & medical detox
Your comprehensive assessment goes far beyond typical intake questionnaires. This process includes laboratory tests to uncover hidden medical complications, comprehensive psychiatric evaluations to understand your mental health landscape, and thorough substance use history assessments that help identify patterns and triggers.
Those lab results often reveal important information - perhaps liver function tests show damage from alcohol use, or blood work indicates nutritional deficiencies affecting mood stability. These findings directly shape both your detox protocol and overall treatment approach.
The psychiatric evaluation requires particular skill because clinicians must untangle which symptoms stem from substance use versus underlying mental health conditions. This detective work takes time and expertise.
Medical detox typically spans 3-7 days, depending on which substances you've been using and your overall health. During this time, withdrawal management might involve medications like benzodiazepines for alcohol withdrawal or buprenorphine for opioid dependency.
Core therapies in an inpatient dual diagnosis track
The therapies used in inpatient dual diagnosis treatment are evidence-based interventions with solid research backing their effectiveness for both addiction and mental health conditions.
Cognitive Behavioral Therapy (CBT) helps you spot and reshape thought patterns that fuel both substance use and mental health symptoms. Dialectical Behavior Therapy (DBT) focuses on building practical skills for managing intense emotions without reaching for substances.
Motivational Interviewing (MI) addresses the internal conflict many people feel about recovery. Trauma-informed therapy recognizes that many people with co-occurring disorders have experienced significant trauma that often underlies both conditions.
Mindfulness-based interventions teach you to observe thoughts and feelings without automatically reacting. Expressive arts therapy provides alternative ways to process emotions that might be too difficult to express in words alone.
Stay updated on the latest developments in evidence-based dual diagnosis approaches through our News Blog.
Medication management & integrated care team
Medication management in dual diagnosis treatment requires a delicate balancing act. Psychiatrists who specialize in addiction medicine understand how psychiatric medications interact with substance use disorders.
Medication-Assisted Treatment (MAT) might play a role in your recovery, particularly for opioid or alcohol addiction. For mental health conditions, your pharmacotherapy might include antidepressants, mood stabilizers, or carefully selected anti-anxiety medications.
Side-effect monitoring becomes particularly crucial because people with co-occurring disorders often show increased sensitivity to medication effects. The integrated care team approach means your psychiatrist, therapist, addiction counselor, and medical doctor communicate regularly about your progress.
Life After Discharge: Aftercare, Family & Outcomes
Leaving inpatient dual diagnosis treatment feels like stepping into a new world. You've stabilized both your addiction and mental health, but now comes the real test - living your recovery in the real world.
The first few months after discharge are the trickiest. Your brain is still healing, and you're learning to handle everyday stress without substances while managing mental health symptoms. This is why having a solid aftercare plan is essential.
Relapse prevention for dual diagnosis looks different than it does for addiction alone. You're not just avoiding substance triggers - you're also watching for signs that your depression is returning or your anxiety is escalating.
Most people benefit from step-down care after inpatient treatment. This might mean spending time in a partial hospitalization program or transitioning to an intensive outpatient program that meets several evenings a week.
Alumni programs from your treatment center can become lifelines. Dual Diagnosis Anonymous and similar support groups focus specifically on managing both addiction and mental health together.

Family therapy often continues long after you leave treatment. Addiction and mental illness affect everyone in the family. Your loved ones need to learn how to support your recovery without enabling old patterns while healing from their own stress and trauma.
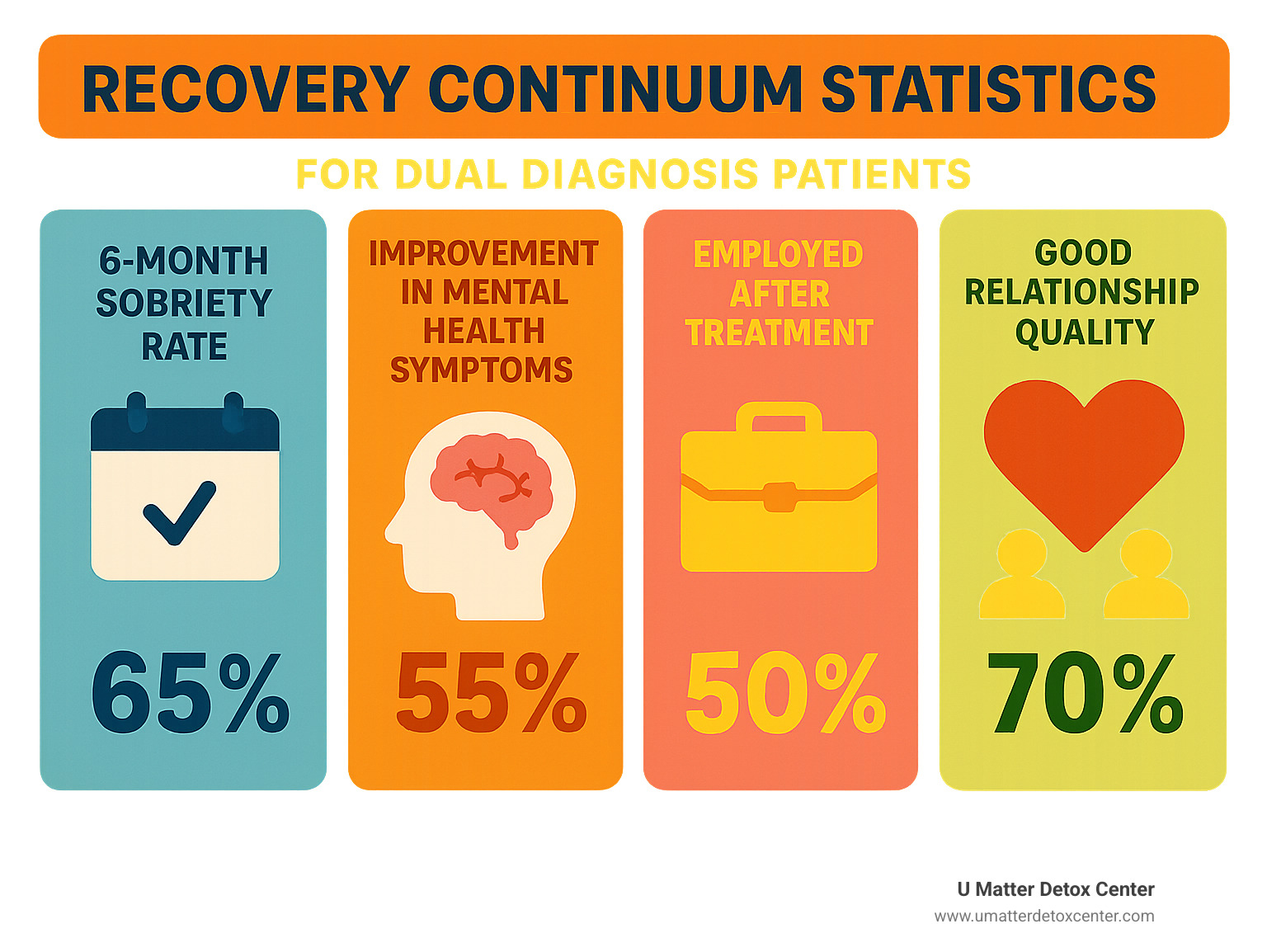
When we look at outcome metrics for inpatient dual diagnosis treatment, success means more than just staying clean and sober. We measure improvements in mental health symptoms, ability to work, relationships, and overall quality of life.
Research shows that people who complete integrated treatment for co-occurring disorders have better long-term outcomes than those who treat conditions separately. You're more likely to maintain sobriety, experience fewer psychiatric hospitalizations, and report better life satisfaction.
Building a support network
Creating your support network after inpatient dual diagnosis treatment is like building a safety net with multiple layers. You need different types of support for different situations.
Peer support forms the foundation of many people's recovery networks. These are friends from treatment, people from support groups, or others in recovery who understand exactly what you're going through.
Sober living homes can provide a perfect bridge between inpatient treatment and independent living. You get your own space but you're surrounded by others committed to recovery.
Telehealth check-ins with your treatment team help maintain connection even when life gets busy. Your professional support team might include a therapist, psychiatrist, and addiction counselor. The key is making sure these professionals communicate with each other.
Building new healthy relationships often means making tough decisions about old friendships. People who only knew you when using substances might not understand or support your recovery.
Choosing & Financing Your Path
Finding the right inpatient dual diagnosis program can feel overwhelming when you're already struggling with both addiction and mental health challenges. But taking time to research your options can make all the difference in your recovery journey.
Facility credentials and accreditation serve as your first quality checkpoint. Look for programs accredited by The Joint Commission or CARF. These organizations put facilities through rigorous evaluations to ensure they meet high standards.
Evidence-based practices should form the backbone of any quality program. When you call facilities, ask specifically about their treatment approaches. Do they use CBT, DBT, and trauma-informed care?

For many professionals, luxury amenities aren't just about comfort - they're about creating an environment where healing can happen without additional stress. At U Matter Detox Center, we understand that your recovery environment matters. Our facilities across Encino, Sherman Oaks, Hollywood Hills, and throughout Los Angeles County combine advanced non-invasive technologies with natural remedies to provide truly individualized care.
The good news about financing is that insurance parity laws work in your favor. These laws require most insurance plans to cover mental health and substance abuse treatment at the same level as medical care.
Finding the right inpatient dual diagnosis center
Location involves more than just convenience. Some people need distance from their usual environment to break old patterns and avoid triggers. Others benefit from staying closer to home for family support.
Consider your specific situation honestly. If your local social circle revolves around drinking, or if your neighborhood has easy access to drugs, treatment farther from home might serve you better.
Program specialties can make or break your experience. Some facilities specialize in treating professionals, understanding the unique pressures and privacy concerns you face.
When researching length of stay options, dual diagnosis typically requires more time than single-condition treatment. Most programs range from 30-90 days, with 60 days being common for complex cases.
Don't be shy about requesting virtual tours or detailed phone consultations. Quality facilities welcome questions and want you to feel confident in your choice.
Costs, insurance & payment options
Understanding your insurance coverage doesn't have to be a nightmare. The Affordable Care Act (ACA) and Mental Health Parity and Addiction Equity Act (MHPAEA) have made treatment much more accessible.
Insurance verification involves a phone call to your insurance company or having the treatment facility check your benefits. You'll want to know your deductible, copayment amounts, any length-of-stay limitations, and whether pre-authorization is required.
Many people are surprised to learn that their insurance covers more than they expected. For those without insurance or with limited coverage, sliding-scale payment options and financing plans can make treatment possible.
When budgeting for treatment, think beyond the initial inpatient stay. Factor in aftercare costs like outpatient therapy, medications, and ongoing support services.
Frequently Asked Questions about inpatient dual diagnosis
How long does inpatient dual diagnosis treatment typically last?
Most inpatient dual diagnosis programs run 30-90 days, with 60 days being the sweet spot for many people. The length depends on how severe both conditions are, how quickly you respond to treatment, your support system at home, and what your insurance covers.
What are the success rates for inpatient dual diagnosis treatment?
Success rates vary depending on how you measure success, but research consistently shows that integrated treatment works better than treating addiction and mental health separately. People who complete inpatient dual diagnosis programs have significantly lower relapse rates and better long-term mental health outcomes.
Who is eligible for inpatient dual diagnosis treatment?
You're typically eligible if you meet diagnostic criteria for both a substance use disorder and a mental health condition, and if outpatient care hasn't worked or isn't safe for you. Factors like suicidal thoughts, severe withdrawal symptoms, multiple failed treatment attempts, or unstable living situations often indicate that inpatient care is necessary.
Conclusion
When you're caught in the exhausting cycle of addiction and mental illness, inpatient dual diagnosis treatment offers a way out. It's not just another treatment option - it's often the lifeline that makes recovery possible when everything else has failed.
The truth is, trying to manage both conditions on your own rarely works. Your brain needs time to heal from both the addiction and the mental health struggles. That healing happens best in a safe place where medical professionals can support you through every step.
At U Matter Detox Center, we've seen people transform their lives through our integrated approach. We don't just treat your addiction or your depression - we treat them together because we know they're connected. Our team combines proven therapies with innovative treatments and natural healing methods that help your mind and body recover simultaneously.
What makes our program different is that we understand you're not just another case number. Whether you're staying at our Beverly Hills location or our Malibu facility, you'll find comfortable, private spaces designed for healing. We work with most insurance plans because we believe everyone deserves access to quality dual diagnosis care.
The research backs up what we see every day - people who get coordinated treatment for both their addiction and mental health do better in the long run. They stay sober longer, feel happier, rebuild relationships, and get their lives back on track.
Maybe you've tried outpatient treatment before and it didn't stick. Maybe you're scared about taking time away from work or family. Those feelings are completely normal. But inpatient dual diagnosis treatment isn't a step backward - it's often the foundation that makes everything else possible.
Recovery isn't just about stopping drug or alcohol use. It's about waking up without crushing anxiety. It's about enjoying time with your family again. It's about feeling like yourself - maybe for the first time in years.
You don't have to figure this out alone anymore. Our team is here to guide you through every part of the process, from your first phone call to your transition back home. We've helped hundreds of people break free from the cycle you're living in right now.
The hardest part is often just picking up the phone. But once you do, you'll find people who understand exactly what you're going through. We know how scary this feels, and we know how to help you through it.
Your life can be different. The person you used to be - or the person you've always wanted to be - is still there. Inpatient dual diagnosis treatment can help you find your way back to them.

