When Military Families Need Dual Diagnosis Support
Dual diagnosis detox covered by tricare is not only possible—it's a comprehensive benefit that many military families don't know they have. If you're struggling with both substance use and mental health challenges, TRICARE offers extensive coverage for integrated treatment that addresses both conditions simultaneously.
Quick Answer: Yes, TRICARE covers dual diagnosis detox through multiple pathways:
- Inpatient detox in hospital settings with 24/7 medical supervision
- Outpatient programs including PHP and IOP for flexible treatment
- Medication-assisted treatment (MAT) for withdrawal management
- Mental health therapeutic services integrated with addiction treatment
- Coverage varies by plan (Prime vs. Select) but benefits are substantial
The reality is stark: according to SAMHSA, about 21.5 million American adults have co-occurring disorders where substance use and mental health conditions feed off each other. For military families, this number is even more concerning due to unique stressors like deployment, trauma, and frequent relocations.
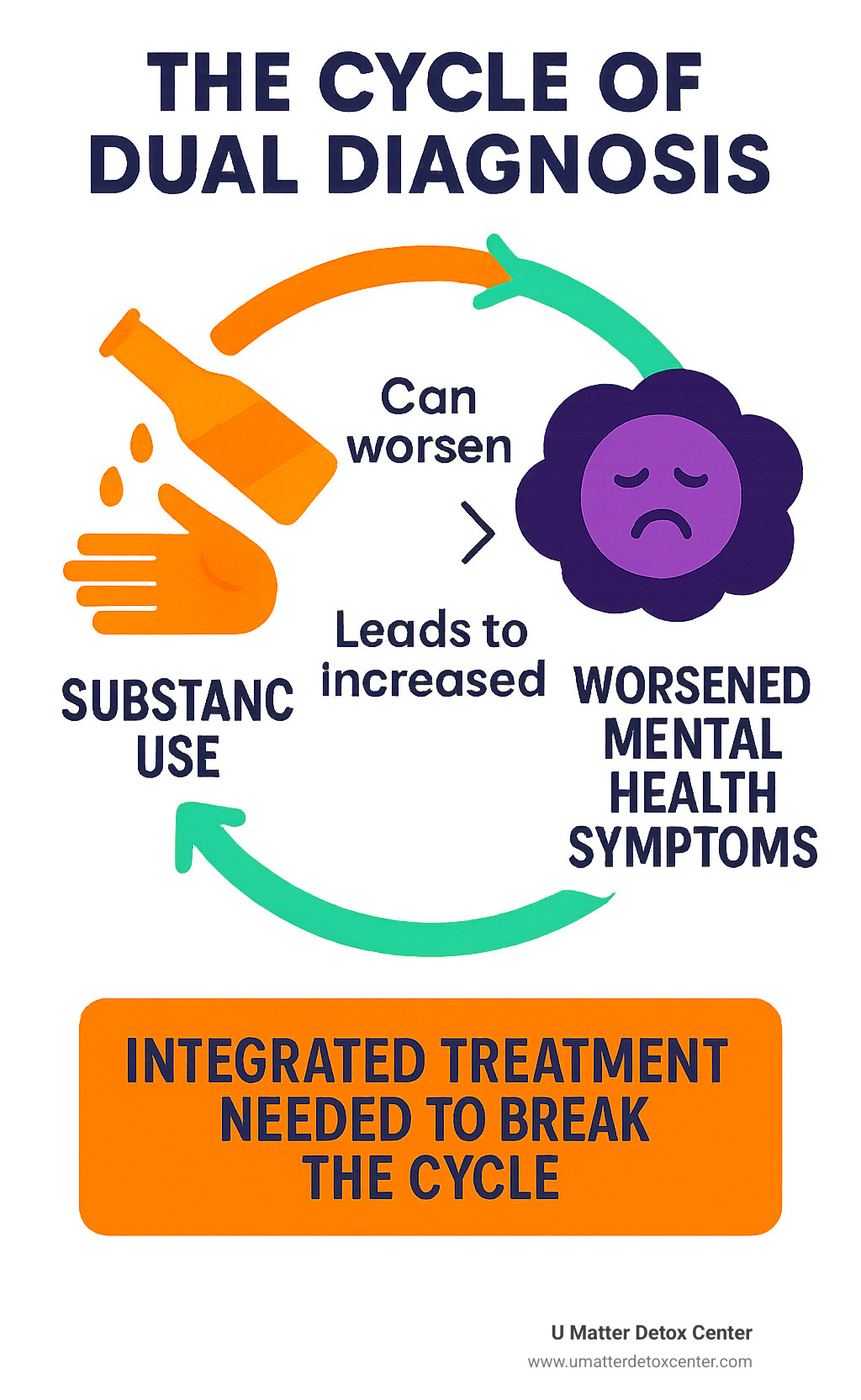
When someone has both addiction and a mental health condition like PTSD, anxiety, or depression, treating just one problem rarely works. The untreated condition often triggers relapse or worsens symptoms. That's why dual diagnosis detox - where both conditions are treated together from day one - has become the gold standard.
TRICARE recognizes this reality. Thanks to the Affordable Care Act and Mental Health Parity laws, your military health benefits now treat mental health and substance use disorders with the same importance as physical health conditions.
Understanding TRICARE's Commitment to Integrated Care
Living with both addiction and a mental health condition is tough enough—navigating insurance shouldn’t add to the stress. TRICARE, the Department of Defense health program that serves about 9.6 million beneficiaries, now treats substance use and mental health disorders as essential health benefits. This parity, required by the ACA and MHPAEA, means integrated dual-diagnosis treatment is a medically necessary service, not a perk.
In practice, that translates into broad coverage for substance use disorder treatment: emergency detox, inpatient or residential care, partial-hospitalization, intensive-outpatient, and continuing therapy—provided the approach is evidence-based and your need is documented.
What Is a Dual Diagnosis?
A dual diagnosis—or co-occurring disorder—exists when a substance use disorder and a mental health condition feed off one another. Typical pairings include:
- Anxiety with alcohol
- PTSD with opioids
- Depression with stimulants
- Bipolar disorder with multiple substances
Success hinges on treating both issues at the same time; focusing on one while ignoring the other nearly always sparks relapse. Integrated teams, not siloed providers, give you the best odds for lasting recovery. (See Mind Meets Matter: Navigating Dual Diagnosis Rehab Programs for details.)
Why Detox Is the Critical First Step
Withdrawal can magnify psychiatric symptoms—alcohol detox may trigger seizures and panic; opioid detox can intensify PTSD; benzodiazepine withdrawal may provoke life-threatening anxiety. That’s why TRICARE covers detoxification: to keep you medically safe while clinicians create a roadmap for long-term care.

What Dual Diagnosis Detox Services Does TRICARE Cover?
TRICARE’s rule of thumb is simple: if a service is medically necessary and evidence-based, it’s probably covered. For dual diagnosis detox that means:
- 24/7 medically supervised detox in hospitals or accredited Residential Treatment Centers
- Structured outpatient care such as Partial Hospitalization (PHP) and Intensive Outpatient Programs (IOP)
- Medication-Assisted Treatment (MAT) with FDA-approved drugs
- Individual, group and family therapy, psychiatric care and after-care planning
Below is a closer look at each level of care—use it as a menu, not a linear checklist.
Medically-Supervised Inpatient Detox
When withdrawal or psychiatric risk is high, inpatient detox offers the safest start. TRICARE funds these stays under Emergency Inpatient Hospital Services. The integrated team can immediately adjust medications if, say, alcohol shakes trigger severe anxiety or opioid detox worsens depression.
For more on what inpatient looks like, see Mind Meets Matter: Understanding Inpatient Dual Diagnosis Programs.
Outpatient Programs: PHP and IOP
Not everyone needs to sleep in a facility. PHP generally runs about six hours a day, five days a week; IOP averages nine hours spread over three to four days. Both programs let you test new coping skills at home and report back for rapid course-correction.
Medication-Assisted Treatment (MAT)

MAT uses medications such as Suboxone, buprenorphine, naltrexone or methadone to blunt cravings and stabilize mood, while concurrent therapy tackles the psychological roots of both disorders. Many of these prescriptions are available without separate prior authorization when written by a TRICARE-authorized provider.
Navigating Your TRICARE Plan for Dual Diagnosis Detox Coverage
Coverage exists; getting it approved often hinges on three variables:
- Plan type (Prime vs. Select)
- Prior authorization and referrals
- In-network vs. out-of-network providers and your share of the bill
TRICARE Prime vs. TRICARE Select
| Feature | TRICARE Prime | TRICARE Select |
|---|---|---|
| Primary Care Manager | Required | Optional |
| Specialty-care referrals | Usually | Rarely |
| Network flexibility | Mostly in-network | In- or out-of-network |
| Out-of-pocket costs | Lower | Higher |
| Prior authorization | Most inpatient | Some services |
| Geographic limits | Near MTF | Broader |
Prime acts like an HMO: start with your Primary Care Manager (PCM), get a referral, and most costs are pre-negotiated. Select behaves more like PPO insurance—greater freedom, slightly higher costs.
In-Network vs. Out-of-Network
Using in-network facilities means TRICARE pays the negotiated rate and you only owe your cost-share. Choose an out-of-network center and you may face up to 15 % above the allowable charge and the hassle of filing claims yourself. Always verify a facility’s status before admission.
Medical Necessity & Prior Authorization
Except for genuine emergencies, TRICARE wants documentation that:
- You have diagnosed co-occurring disorders
- Outpatient care would be insufficient
- The facility is TRICARE-authorized
Your provider submits this information; once approved, coverage is locked in for the authorized stay.
How to Find and Access a TRICARE-Approved Dual Diagnosis Detox Center

Finding help is a two-step process: locate an approved provider, then complete admissions paperwork.
Step 1: Locate a Provider
- Use TRICARE’s Find a Doctor tool.
- Filter by “Substance Use Disorder” and “Mental Health” to see dual-diagnosis facilities.
- Confirm the center accepts your specific TRICARE plan (Prime or Select).
- If you’re stuck, call member services; they will walk you through options in the East, West or Overseas region.
Key questions to ask the admissions team:
- Do you treat co-occurring disorders?
- Which levels of care do you offer (detox, PHP, IOP)?
- Is prior authorization needed for my stay?
- What out-of-pocket costs should I expect?
Step 2: What Happens After You Call
Comprehensive assessment: medical history, psychiatric evaluation, substance-use timeline.
Individualized plan: detox protocol, medication schedule, therapy lineup, family involvement.
24/7 monitoring: to manage withdrawal complications and mental-health flare-ups.
After-care planning: transition to inpatient rehab, PHP/IOP, or outpatient therapy plus community support.

Frequently Asked Questions about Dual Diagnosis Detox Covered by Tricare
What are the main eligibility criteria?
- Documented diagnoses of a substance use disorder and a mental health condition
- Provider statement that integrated detox is medically necessary
- Referral and/or prior authorization (Prime usually requires a PCM referral; Select often does not)
- Functional impairment that makes a lower level of care unsafe
Does TRICARE cover medications like Suboxone?
Yes. FDA-approved medications—including Suboxone, buprenorphine, naltrexone and methadone—are covered when prescribed by a TRICARE-authorized clinician and paired with counseling.
Are any substance-use treatments not covered?
TRICARE excludes interventions that are unproven or potentially harmful, such as aversion therapy with electric shock or experimental treatments lacking scientific support. Covered care must be evidence-based, medically necessary and delivered by TRICARE-authorized providers.
Conclusion: Your Path to Integrated Recovery Starts Here
Recovery from dual diagnosis isn't just a distant hope—it's a real, achievable goal that thousands of military families have reached with TRICARE's comprehensive support. The journey forward begins with understanding that dual diagnosis detox covered by tricare is more than just a benefit—it's your earned right to quality healthcare that addresses both your addiction and mental health needs together.
Throughout this guide, we've explored how TRICARE's commitment to integrated care means you never have to choose between treating your substance use disorder or your mental health condition. The coverage is genuinely comprehensive, spanning from emergency detox services to long-term therapeutic support, with flexible options for inpatient treatment, outpatient programs, and medication-assisted treatment that work together to address both conditions simultaneously.
What makes TRICARE's approach so effective is its recognition that dual diagnosis isn't two separate problems—it's one complex condition that requires coordinated care. Whether you're struggling with PTSD and alcohol use, anxiety and prescription drug dependence, or depression and substance abuse, TRICARE provides a clear pathway to recovery that honors your service and supports your entire family.
The most important step is often the hardest one: reaching out for help. But remember, you've already taken the first step by reading this guide and learning about your options. That shows strength, not weakness.
At U Matter Detox Center, we understand the unique challenges facing military families. Our luxury, holistic approach to dual diagnosis detox combines advanced non-invasive technologies with natural remedies, creating a healing environment that goes beyond traditional treatment methods. We're experienced in working with TRICARE insurance and can help you steer both your recovery and your benefits, ensuring you receive the comprehensive care you deserve without the stress of insurance complications.
Your service to our country has earned you access to quality healthcare, including dual diagnosis treatment. Don't let uncertainty about coverage or fear of stigma prevent you from getting the help you need and deserve. The path to recovery is clearer than you might think, and TRICARE is designed to support you every step of the way.
Take the first step today and find comprehensive and compassionate care for co-occurring disorders that addresses both your addiction and mental health needs with the respect and expertise you deserve.
Remember: seeking help demonstrates courage and commitment to your recovery and your family's wellbeing. Your path to integrated recovery starts with a single phone call or click. TRICARE is ready to support you, and so are we. You matter, your recovery matters, and help is available right now.

